- What is 93306 CPT Code and Why It Matters in 2025
- Key Components Included in CPT Code 93306
- Clinical Scenarios Where CPT 93306 Is Used
- Real-World Applications of CPT Code 93306
- Modifier Usage and Documentation Guidelines for CPT 93306
- Common Billing Errors and Compliance Risks in 93306 Reporting
- Avoiding Denials Through Compliance-Driven Processes
- Reimbursement Insights and Payer Trends for CPT 93306 (2025)
- Key Factors That Influence 93306 Reimbursement
- How to Prevent Denials and Strengthen Claim Accuracy for CPT 93306
- Workflow Tips for Clean 93306 Claim Submission
- CPT 93306 vs. Related Echocardiogram Codes—Knowing When to Use Which
- Why Proper Code Selection Matters
- Documentation & Compliance Best Practices for CPT 93306 (2025 Edition)
- Frequently Asked Questions (FAQ) About CPT 93306
- Final Thoughts—The Bottom Line on CPT 93306 Accuracy
The 93306 CPT code is one of the most important billing codes in cardiology; however, it is frequently not well understood. If you lack the appropriate knowledge on how to document, code, and submit echocardiology claims correctly, your organization may be significantly underpaid for these services or, worse, not get paid at all!
Designed for U.S. Providers, this comprehensive guide describes CPT 93306 from a clinical and billing standpoint. You will learn its definition, when to use it, which modifiers to attach, and payer rules. Let’s decode the heartbeat of accurate echocardiogram billing.
What is 93306 CPT Code and Why It Matters in 2025
The code 93306 is for a full transthoracic echocardiogram, which is a noninvasive test that uses ultrasound to create pictures of the heart in real time. This report comprises a 2D image, spectral Doppler and color flow Doppler. For 2025, this code still serves as a foundation to our cardiovascular diagnostics and reimbursement integrity in medical billing.
From a clinical perspective, CPT 93306 represents an inclusive evaluation of the heart’s structure, valve function, and blood flow. For billing purposes, it describes the entire range of work that’s included—technical and professional, in other words. Accurate usage ensures accurate payouts, prevents denials, and maintains compliance with AMA and Medicare policies.

Key Components Included in CPT Code 93306
CPT 93306 combines multiple necessary diagnostic components for an accurate evaluation of the heart. It involves 2D echocardiographic images that provide pictures of heart anatomy, spectral Doppler to measure the velocity of blood flow, and color flow Doppler to see turbulence and direction. These elements combine to provide a comprehensive assessment of heart function for both clinical validity and billing purposes.
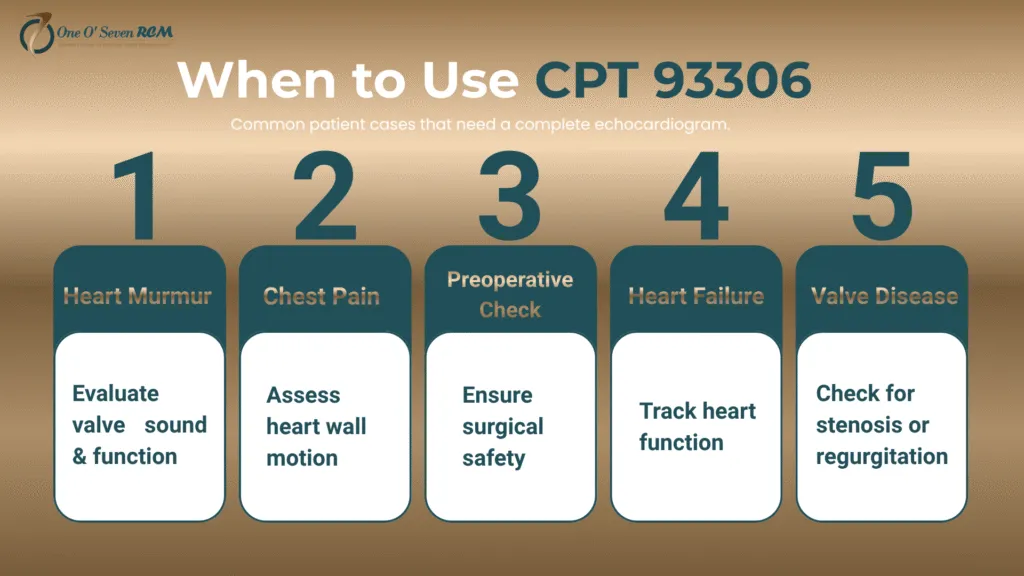
Clinical Scenarios Where CPT 93306 Is Used
The 93306 CPT Code is essential in the care of various cardiac diseases. It is employed when providers require a complete transthoracic echocardiogram to determine chamber size, wall motion, or valve integrity. This code records detailed cardiac information required for patient management and verification of disease progression.
Physicians all over the USA depend on CPT code 93306 for heart murmurs, valvular disease, chest pain or even preoperative cardiac clearance. All of the use cases represent a justified medical need for remuneration. Accurate documentation shows payers that the service had clinical value—making it more likely they’ll avoid rejecting claims and continue to provide your practice with a revenue stream.
Real-World Applications of CPT Code 93306
Consider a patient who arrives with unexplained chest pain. The provider requests additional images of the heart to evaluate its structure as well as how well blood is flowing through it (a complete echocardiogram). It is all-inclusive. 93306 captures all technical and interpretive elements. When applied properly, it supports medical necessity, clean claims and compliance with CMS and AMA coding rules.
Common Clinical Use Cases for 93306 CPT Code
| Clinical Scenario | Purpose of Echocardiogram | Why CPT 93306 Applies |
| Heart Murmur | Detects abnormal valve sounds and function. | A full 2D+ Doppler study is required. |
| Chest Pain | Evaluates heart wall motion, flow, and chamber health | Confirms or rules out cardiac origin |
| Preoperative Cardiac Evaluation | Ensures surgical safety for high-risk patients | Provides a complete cardiac functional report |
| Heart Failure Monitoring | Tracks ventricular function and response to therapy. | Longitudinal follow-up using a full echo study |
| Valve Disease | Identifies stenosis or regurgitation severity | Requires Doppler and color flow for assessment |
Modifier Usage and Documentation Guidelines for CPT 93306
Applying the correct CPT 93306 modifiers ensures your claims reflect the exact service rendered. Modifiers like 26 (professional component) and TC (technical component) separate physician interpretation from equipment use. Others—59, 76, and 77—clarify distinct, repeated, or multi-provider services. Proper modifier use prevents payer confusion and protects against partial reimbursements.
Accurate documentation remains the backbone of echocardiogram billing. Each report must outline structures examined, Doppler findings, and clinical necessity. Missing details lead to claim denials and compliance risk. Align your reporting with AMA CPT and Medicare LCDs to substantiate medical necessity while maintaining full transparency in diagnostic interpretation and claim integrity.
Essential Modifiers That Support CPT 93306
Modifiers reveal the scope of services delivered under CPT 93306. For example, use 26 for physician interpretation only or TC for billing for technical execution. Apply 59 for distinct procedural service and 76/77 for repeat testing. Always pair modifiers with proper notes to satisfy payer audit requirements.
Key Modifiers and Their Application
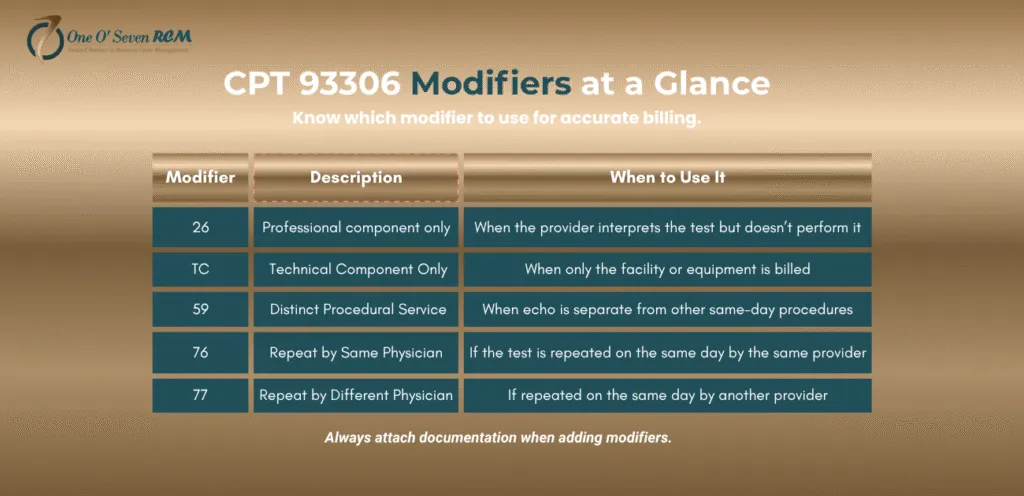
| Modifier | Description | When to Use It |
| 26 | Professional component only | When the provider interprets the test but doesn’t perform it |
| TC | Technical component only | When only the facility or equipment is billed |
| 59 | Distinct procedural services | When echo is separate from other same-day procedures |
| 76 | Repeated by the same physician | If the test is repeated on the same day by the same provider |
| 77 | Repeat by a different physician | If repeated on the same day by another provider |
Common Billing Errors and Compliance Risks in 93306 Reporting
Even the most skilled coders sometimes receive rejections when they bill for the 93306 CPT Code. Common mistakes are a lack of documentation for the Doppler, pairing too many modifiers, or up-coding that is limited to completion. Such errors not only stall payments but can also invite scrutiny in payer audits and result in costly fines.
Compliance demands accuracy, not assumptions. All echocardiogram studies must report medical necessity and provide ICD-10 codes to substantiate this need in accordance with payer-specific documentation requirements. “Over-documentation, such as cut-and-paste templates, can be warning signals of potential non-compliance and should be minimized.” Mandatory workflow and account auditors help reduce claim denials significantly while keeping your billings up to date.
Avoiding Denials Through Compliance-Driven Processes
Conducting pre-submission proactive compliance checks reduces the risks of denial. Use claim scrubbers to identify incomplete CPT 93306 entries, cross-check modifiers based on payer guidelines, and confirm clinical notes back up the procedure. This data-driven policing prevents dirty claims and creates a defensible audit trail for each submitted echocardiogram claim.
Reimbursement Insights and Payer Trends for CPT 93306 (2025)
Payment for 93306 CPT Code. There is no uniform coverage and payment specific to the 93306 CPT code based on payer contracts, facility type, and place of service. Medicare’s national 2025 average reimbursement for a full transthoracic echocardiogram is $210-240. Yet private insurers could be paying more for compliant documentation with Doppler and full anatomic interpretations.
Maximize reimbursement by capturing and documenting all required components of the procedure. Excluding a single Doppler or M-mode could result in a down-coding to 93307/93308, thereby reducing the repayment loss by approximately 30%. By quarterly reviewing payer policies, practices can stay on top of shifting payer reimbursement trends and prevent payment discrepancies.
Key Factors That Influence 93306 Reimbursement
Multiple factors influence the ultimate reimbursement for CPT 93306 – such as geographically specific fee schedules, responsible appending of modifiers, and network participation. Hospital-based providers may experience lower per-claim payments resulting from facility cuts, while independent practices are often paid higher global rates by billing the professional and technical components in-house.
How to Prevent Denials and Strengthen Claim Accuracy for CPT 93306
CPT 93306 Denials can be Avoided at the First Place with Precision. Make sure all Clinical findings, Dopplers, and interpretations match the payer’s documentation requirements. Leaving out modifiers, incomplete studies, or nebulous notes can turn legitimate echocardiogram claims into wasteful billing-time denials. Consistency and adherence help maintain predictability in your reimbursement process.
Accuracy begins before submission. Remember to check patient eligibility, medical necessity and CPT/ICD-10 combinations. Claim scrubbing software utilized by practices identifies documentation omissions prior to the occurrence of claims errors. The objective is obvious—get cleaner claims out the door, eliminate administrative lag time, and get paid sooner by Medicare and commercial insurers.
Workflow Tips for Clean 93306 Claim Submission
A proactive process leads to Seamless Echocardiogram billing. Teach your billing personnel to verify all elements of a TTE, renegotiate payer fee schedules with quarterly updates, and specify the use of Doppler. Routine internal monitoring, combined with denial tracking, forms a closed-loop process that enhances claims accuracy and fortifies revenue cycle strength with every payer.
CPT 93306 vs. Related Echocardiogram Codes—Knowing When to Use Which
Understanding the distinctions between CPT 93306 and its related echocardiogram codes prevents underpayments and denials. Each code represents a different level of diagnostic detail. Using 93306 for an incomplete study can lead to audits or down-coding, while underreporting a complete study as limited can cause lost revenue opportunities.
Comparison of Echocardiogram CPT Codes
| CPT Code | Description | Includes | When to Use |
| 93306 | Complete transthoracic echocardiogram | 2D imaging, M-mode, spectral Doppler, color flow Doppler | For a full study of heart structure and function |
| 93307 | Complete echo without Doppler | 2D imaging only | When Doppler is not performed or is not medically necessary |
| 93308 | Limited or follow-up echo | Partial 2D imaging | Used for follow-up exams or single-focus evaluations |
| 93320 | Doppler echo, complete | Spectral Doppler only | Used as an add-on when Doppler is done separately |
| 93321 | Doppler echo, limited | Partial spectral Doppler | For limited velocity flow studies |
| 93325 | Color flow velocity mapping | Color Doppler only | Add-on when color Doppler is performed separately |
Why Proper Code Selection Matters
Choosing the right echocardiogram code ensures compliance, full reimbursement, and audit protection. Overstating or understating service complexity can trigger denials. Document each component clearly—2D, M-mode, spectral, and color Doppler—to justify 93306. Coders who maintain this accuracy strengthen both the clinical narrative and financial outcomes for every cardiology practice.
Documentation & Compliance Best Practices for CPT 93306 (2025 Edition)
Strong documentation transforms clean claims into consistent payments. On every CPT 93306 report, there would be a list of “interrogated structures”– ventricles, valves, atria, aorta and pericardium—and an indication that Doppler and color flow studies were performed. Missing notes often result in down-coding or denials, so delivering accurate reports also protects your revenue and compliance history.
Compliance in 2025 requires real-time accuracy. Get your documentation in line with Medicare LCDs and the AMA CPT® guidelines to satisfy payers’ expectations. For each report, provide measurements, interpretations, and a statement of medical necessity. Practices that integrate checklists for clinical completeness experience fewer post-payment audits and significantly higher reimbursement reliability across payers.
Key Compliance Checklist for 93306 Documentation
Before submitting a claim, confirm each of these points: (1) a complete transthoracic echo was performed, (2) both Doppler components are documented, (3) images are stored with timestamps, (4) clinical necessity is noted, and (5) the provider’s signature and interpretation are included. These elements form your compliance foundation.
Frequently Asked Questions (FAQ) About CPT 93306
What is included in CPT 93306?
Its description covers a complete transthoracic echo that uses 2D imaging and M-mode (which includes spectral Doppler) along with color flow Doppler, enabling a thorough assessment of the heart’s structure and blood flow.
Will CPT 93306 allow for modifiers?
That should be a separate technical and professional fee using modifier 26 for the professional part and TC for the technical portion; modifiers 59, 76 and 77 apply if it’s a new or repeated procedure—they’re also very important in order to correctly code CPT code 93306 reimbursement.
What are the frequently encountered denials of the CPT 93306 claim?
There are denials due to missing Doppler documentation, wrong modifier selection, or inappropriate ICD-10 codes; verifying every CPT 93306 element would save providers from rejections and compliance in cardiology billing.
What is the frequency of billing for CPT 93306?
Medicare will usually cover one full echocardiogram per year unless you can justify having more than this; then you must ensure that modifiers 76 or 77 are appropriately used so that the claim will not be denied.
Final Thoughts—The Bottom Line on CPT 93306 Accuracy
Mastering CPT 93306 is more than billing—it’s about ensuring diagnostic accuracy and protecting your bottom line. Each clean claim reflects operational excellence, while every error risks unnecessary write-offs. By aligning coding, modifiers, and compliance together, healthcare providers create sustainable revenue streams and stronger financial outcomes in 2025 and beyond.
At One O Seven RCM, we help providers decode complex cardiology billing and maintain claim precision with unmatched expertise. Our approach simplifies reimbursement for echocardiography CPT codes, improves first-pass claim success, and strengthens compliance so your focus stays on patients—not payer paperwork.
Want cleaner claims and fewer denials? Discover how One O Seven RCM’s data-driven billing solutions can help your practice master CPT 93306 and every cardiology reimbursement challenge.
Related Reading:
Explore CPT 90834 — A Complete Guide for Mental Health Billing for more insights into accurate coding practices.