Another CO-97 denial. Another claim sitting in your rejection pile. Another hour your team will spend figuring out what went wrong.
If you’re seeing CO-97 show up on your remittance advice more than once a month, this isn’t random bad luck. It’s a pattern. And that pattern points to a workflow gap that’s costing your practice more than you think.
This guide breaks down exactly why CO-97 denials keep targeting your claims, the root causes behind them, and how to stop them for good.
What CO-97 Actually Means (30-Second Explainer)
The CO-97 denial code is Claim Adjustment Reason Code 97. The official co 97 denial code description from payers reads: “The benefit for this service is included in the payment/allowance for another service/procedure that has already been adjudicated.”
What does CO-97 mean in plain English? Simple: the payer thinks you already got paid for this service as part of something else. They’re saying the service is bundled into another procedure.
The “CO” prefix stands for Contractual Obligation. That means this is your write-off, not the patient’s responsibility. But here’s what most practices miss: CO-97 denials are often wrong. When they’re wrong and you don’t challenge them, you’re leaving money on the table every single time.
The Hidden Cost of Ignoring CO-97 Denials
Most practices focus on the denied amount when they see a CO-97 denial. That’s a mistake. The real denial cost is what you spend trying to fix it.
Reworking a CO-97 denial costs $25 to $118 in staff time alone. That includes reviewing the claim, checking documentation, researching bundling rules, and resubmitting. One claim doesn’t sound like much. But these denials rarely come alone.
What usually happens: you get one denial, then realize the same error hit 10 other claims that week. Same procedure pair. Same missing modifier. Same workflow gap nobody caught before submission.
Here’s where denial cost compounds into revenue loss. Your team spends hours fixing preventable errors. Some claims never get resubmitted because the dollar amount doesn’t justify the effort. That’s revenue loss you can’t recover.
THE CO-97 MATH:
- Average denial rework cost: $25 to $118 per claim
- If you’re getting 10 CO-97 denials per month: $250 to $1,180 in rework costs alone
- Add in lost revenue from claims that never get resubmitted
- Annual impact for a mid-size practice: $15,000 to $50,000+
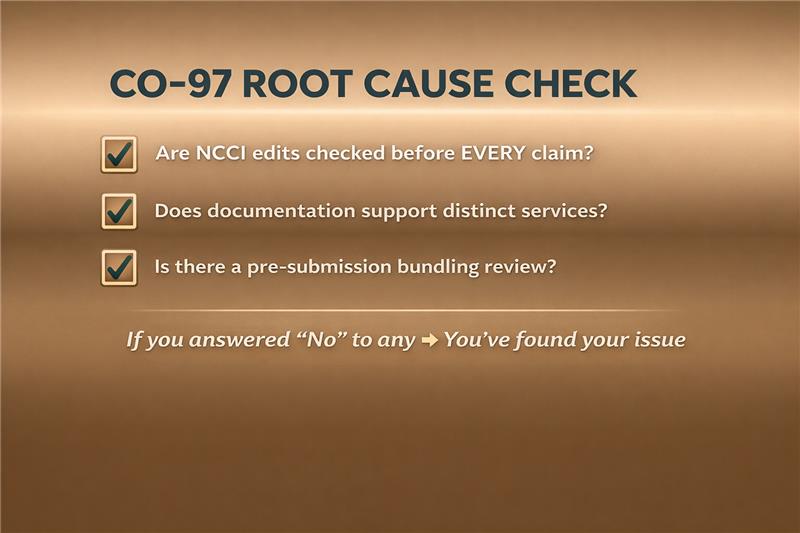
Why CO-97 Keeps Happening: The 3 Root Causes
Most articles list five to eight causes for CO-97 denials. But they’re listing symptoms, not root problems. Every CO-97 denial code reason I’ve seen in 15 years of billing work traces back to one of three workflow gaps.
Fix these three root causes, and you’ll stop most bundled procedures denials before they happen.
Root Cause #1: Your Verification Process Has Gaps
CO-97 happens because nobody checked the bundling rules before the claim went out. This isn’t a coding error. It’s a workflow gap.
If your billers are submitting claims without verifying NCCI edits first, you’ll keep getting hit with the same denials. The code pair that denied today will deny again next week when the same procedure combination goes out.
The issue is process, not people. Your team can’t check what they don’t have time to check. When claims go straight from charge entry to submission without a bundling review step, denials are inevitable.
Root Cause #2: Your Documentation Doesn’t Support Separate Billing
Even when services are actually distinct, the claim will deny if documentation doesn’t show why they’re separate. Modifiers only work when the chart backs them up.
Here’s what usually happens: The provider performs two procedures at different sites or during separate sessions. Your coder adds modifier 59 because the services weren’t bundled. The payer denies it anyway because the operative note doesn’t clearly document the distinction.
Documentation drives the denial outcome. Without clear evidence that services were truly separate, no modifier will save that claim.
Root Cause #3: You’re Reactive, Not Proactive
If you’re only dealing with CO-97 after the denial arrives, you’re always behind. Why CO-97 happens repeatedly at the same practices: they fix individual claims instead of fixing the system that created them.
Practices with low denial rates build prevention into their submission workflow. They catch bundling issues during claim scrubbing, not after the remittance advice comes back. That’s the difference between managing denials and preventing them.
Got a CO-97 Denial? Follow This Decision Tree
You don’t need a manual to resolve CO-97 denials. You need a decision tree that tells you exactly what to check and when to stop digging.
This co 97 denial solution flowchart walks you through the diagnosis in the same order I’d use if you called me with a denial in your hand. Two questions determine how to fix co 97 denial: same-day bundling or global period issue?
START: You received CO-97 denial
↓
QUESTION 1: Were two procedures billed on the same date?
→ YES: Go to BUNDLING CHECK
→ NO: Go to GLOBAL PERIOD CHECK
BUNDLING CHECK:
Are codes paired in NCCI edits?
→ YES + Modifier Indicator = 0: Write off (truly bundled)
→ YES + Modifier Indicator = 1: Can you document distinct services?
→ YES: Add modifier 59/X-modifier, resubmit
→ NO: Write off
→ NO: Appeal—payer error
GLOBAL PERIOD CHECK:
Is service within 10/90-day surgical window?
→ YES: Is it unrelated to original surgery?
→ YES: Add modifier 79, resubmit
→ NO: Included in global—write off
→ NO: Appeal—payer error
END RESULT: Resubmit, Appeal, or Write Off
Every path in this tree leads to one of three outcomes: resubmit with the right modifier, appeal because the payer’s wrong, or write it off and document why.
Most denials resolve at the NCCI check. If modifier indicator equals zero, the codes are truly bundled and can’t be separated. If it equals one, documentation determines whether you can bill separately.
The key is knowing when to stop. If you can’t support separate billing with documentation, don’t resubmit. Fix the documentation gap for next time and move on.
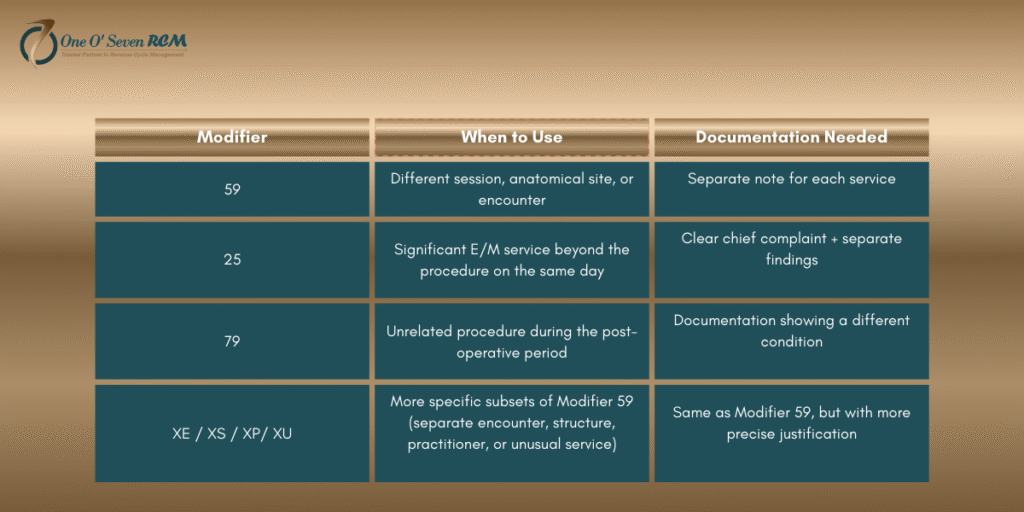
Modifiers Won’t Save You (Unless You Use Them Right)
Slapping modifier 59 on a claim doesn’t fix unbundling issues. It creates new problems, especially when auditors start digging.
The Modifier 59 Trap
Modifier 59 is the most overused and most audited modifier in medical billing. The OIG has specifically flagged modifier 59 abuse in multiple reports. When practices use it as a default response to every bundling denial, they’re not solving the problem. They’re inviting scrutiny.
Using modifier 59 without documentation support is a compliance risk. Payers know it gets misused. That’s why many now require the more specific X-modifiers (XE, XS, XP, XU) that force you to explain exactly why services were distinct.
When Modifiers Actually Work
Modifiers work when three conditions are met: documentation clearly shows distinct services, the NCCI modifier indicator equals one, and you can defend the claim in an audit.
Without those three elements, adding a modifier just delays the inevitable denial. Here’s what each common unbundling modifier actually requires:
Which Payers Hit You Hardest with CO-97?
Not all payers apply bundling rules the same way. If you’re tracking your CO-97 denials by payer, you’ll start seeing patterns that point to specific workflow fixes.
The co 97 denial code Medicare triggers most often come from strict NCCI enforcement and global period violations. Medicare doesn’t bend on these rules. Commercial payers have their own quirks. The co 97 denial code BCBS issues often stem from proprietary edits that go beyond standard NCCI tables.
Here’s where pattern recognition matters: run a report on your last 90 days of CO-97 denials. Sort by payer. What you find tells you exactly where to focus.
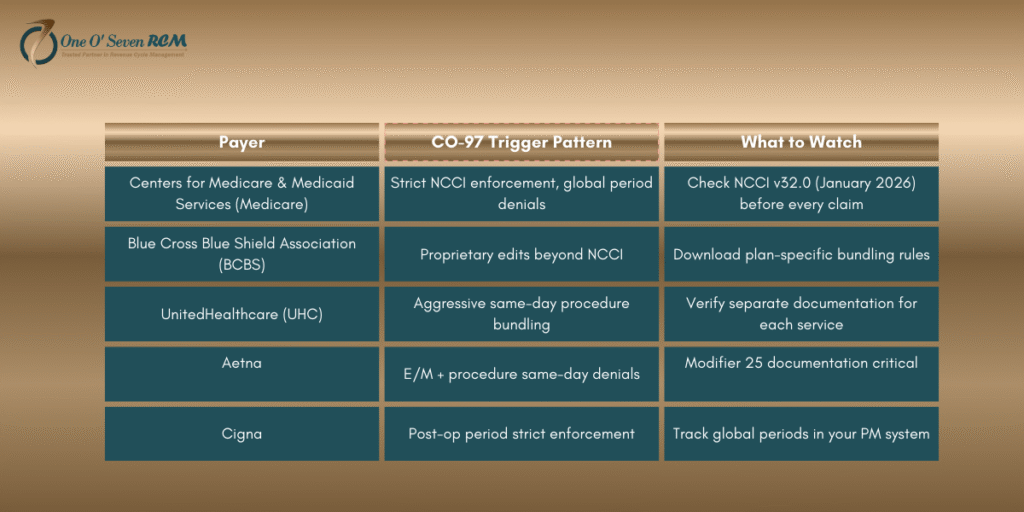
PATTERN CHECK: If 60%+ of your CO-97 denials come from ONE payer,
you have a payer-specific workflow gap, not a general coding problem.
That insight changes everything. A medicare denial code co 97 concentration means your NCCI verification step needs work. Heavy BCBS denials? You’re missing their proprietary edit rules entirely.
What’s Changed in 2026 (And What Hasn’t)
The NCCI edits update quarterly. If you’re not checking the latest version before submitting claims, you’re working with outdated bundling rules.
What’s New in 2026:
The January 2026 NCCI edits (version 32.0) brought several changes that affect CO-97 denial rates:
- Audiology code bundling: New pairs affect ENT and audiology practices
- COVID-19 vaccine admin fix: CMS corrected an error with CPT 90480 bundling. If you got denials on this code in 2025, appeal them now
- AI-augmented analysis codes: New bundling restrictions on these procedure codes
The CMS updates for 2026 also include TEAM Model expansion. Bundled payments now cover Lower Joint Replacement, Spinal Fusion, CABG, and Major Bowel procedures. Services billed within the 30-day episode window may deny as CO-97 even when they’d normally pay separately.
[IMPORTANT BOX PLACEMENT: Insert after the changes section]
Don’t chase definition changes. Focus on keeping your NCCI edits current and understanding new bundled payment models as they roll out.
The 15-Minute CO-97 Response Protocol
When a CO-97 denial lands on your desk, you shouldn’t need an hour to work it. This co 97 denial solution protocol gets you from confusion to decision in 15 minutes flat.
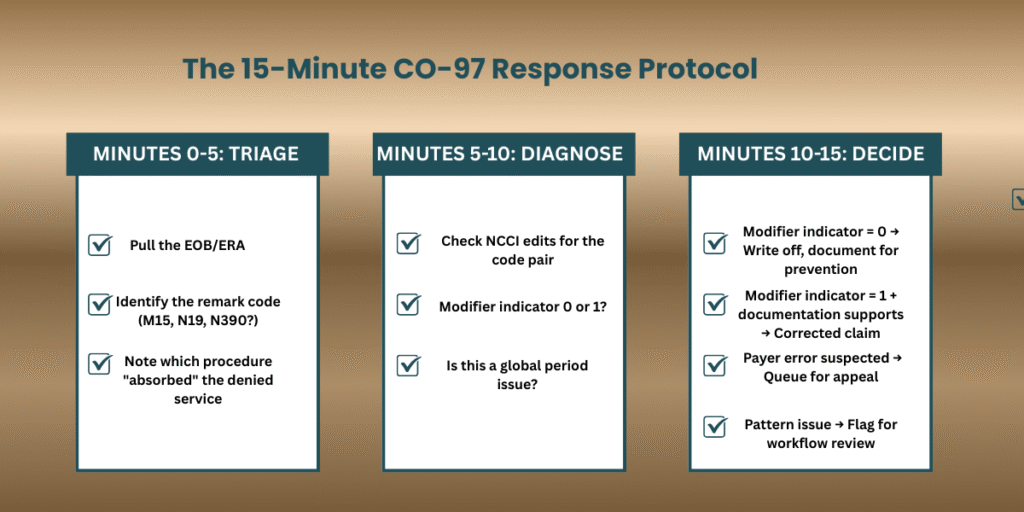
Here’s how to resolve co 97 denial code issues without spinning your wheels. The first five minutes are triage: pull the EOB, find the remark code, and identify which procedure absorbed the denied service.
Minutes five through ten are for diagnosis. Check NCCI edits for that code pair. The modifier indicator tells you everything. Zero means truly bundled, and you can’t fix CO-97 no matter what modifier you add. One means documentation might support separate billing.
The final five minutes: decide and act. Resubmit if you can fix CO-97 with proper documentation. Queue for appeal if the payer made an error. Write it off if it’s truly bundled, but log the pattern to prevent future denials.
That’s how to resolve co 97 denial code problems in a quarter hour. The real co 97 denial solution is a repeatable process, not extra effort on every claim.
Most CO-97 denials can be triaged in 15 minutes.
If your team is spending longer, they need a better system, or better support.
Stop CO-97 Before It Starts: The 3-Layer Prevention System
Fixing denials costs more than preventing them. A real denial prevention system catches bundling issues before claims go out, not after they come back denied.
Here’s the three-layer approach that works to prevent CO-97 denial at your practice.
Layer 1: Pre-Claim Verification
Check NCCI edit status for procedure pairs before any claim leaves your office. Build this step into your workflow, not as an afterthought when denials pile up.
Implementation: Use claim scrubbing software with current NCCI tables. These tables update quarterly, so make sure your system stays current.
Layer 2: Documentation Standards
Establish clear documentation requirements for services commonly billed together. When providers know what’s needed upfront, you won’t chase notes after the fact. This is how you prevent bundling denials at the source.
Implementation: Create specialty-specific bundling cheat sheets. Post them where providers can reference them during documentation.
Layer 3: Pattern Monitoring
Track CO-97 by payer, provider, and procedure code monthly. Patterns reveal workflow gaps before they become expensive. This layer of denial prevention catches systemic issues that individual claim reviews miss.
Implementation: Build a monthly denial dashboard with CO-97 breakdown. Spotting trends early is the easiest way to prevent CO-97 denial before it happens.
CO-97 Denial Code: Your Questions Answered
Q1: Why do I keep getting CO-97 denials for the same codes?
Recurring CO-97 denials for the same code pairs point to a workflow gap, not random errors. Check if your team verifies NCCI edits before submission. If they’re not checking, the same bundling trigger will hit every claim with that procedure combination.
Q2: Is CO-97 my fault or the payer’s fault?
It depends on the situation. If NCCI edits clearly bundle the codes and no modifier applies, the denial is correct. When your documentation supports distinct services but a modifier was missing, that’s a correctable error on your end. If the payer applied bundling rules incorrectly, it’s their mistake. Appeal it.
Q3: How long do I have to appeal a CO-97 denial?
Timely filing limits vary by payer. Most allow 90 to 180 days for appeals. Medicare gives you 120 days for redetermination requests. Check your specific payer contract for exact deadlines, and don’t wait until the last week to file.
Q4: Can CO-97 denials be automatically prevented?
Yes, with the right claim scrubbing software. Modern RCM systems check NCCI edits before submission and flag bundling issues automatically. Without automation, you’re relying on manual review. Manual review misses things, especially when your team is busy.
Q5: What’s the difference between CO-97 and CO-4?
CO-97 means the service is bundled into another procedure’s payment. CO-4 means a modifier is missing or invalid. Here’s the connection: CO-4 is often the fix for CO-97. Adding the right modifier can turn a bundled denial into a payable claim.
Q6: Does CO-97 affect my payer contracts?
High denial rates can impact contract negotiations and payer relationships. Some payers track denial patterns across their network. Practices with frequent bundling issues may face increased scrutiny or less favorable terms at renewal time.
Q7: Should I use modifier 59 or XE/XS/XP/XU?
CMS prefers the X-modifiers as more specific alternatives to modifier 59. That said, many commercial payers still accept 59 without issue. Check payer preference first, but always ensure your documentation supports whichever modifier you choose.
Q8: What if I disagree with the NCCI bundling rule?
You can’t dispute NCCI edits themselves. They’re CMS policy. But if your specific clinical situation is an exception, document it thoroughly and use the appropriate modifier. If the payer still denies after that, appeal with clinical justification explaining why services were distinct.
Q9: How do I track CO-97 denial patterns?
Run a monthly report filtering by denial code CO-97. Break down results by payer, provider, and procedure code. Look for concentrations. When 60% of your CO-97 denials come from one source, that’s where your workflow gap lives.
Q10: When should I just write off a CO-97 denial?
Write off when the NCCI modifier indicator equals zero, when services truly were bundled with no documentation supporting separation, or when the dollar amount doesn’t justify rework time. But always log the write-off. That data helps you spot prevention opportunities.
CO-97 Denials Are a Symptom—Fix the System
CO-97 denials aren’t random. They’re signals that something in your revenue cycle needs attention, whether it’s verification, documentation, or follow-up.
The practices that eliminate CO-97 denial issues don’t do it by working harder on individual claims. They fix the underlying workflow problems. Building prevention into your system beats fighting the same denials month after month.
If you’re spending more time fighting denials than preventing them, it’s time to fix the system, not just the claims.
One O Seven RCM specializes in identifying denial patterns and building prevention systems that work. We don’t just fix claims; we fix workflows. [Get your free denial pattern analysis] and see exactly where your CO-97 issues are coming from.
Last Updated: January 2026
Reviewed by Andrew Christian, CPC, a denial management specialist at One O Seven RCM with 12 years of experience in healthcare revenue cycle optimization.
This guide reflects NCCI edits version 32.0 (effective January 1, 2026). Bundling rules update quarterly. Verify current edits before claim submission.

