- What Is Time-Based Coding, and Why Does It Matter for Providers?
- CPT 2025 Time-Based Guidelines: How Time Is Calculated
- CPT Time Threshold Table (2025 Update)
- How Total Time Is Counted (and What Isn’t)
- Time-Based Coding vs. MDM: When to Use Which
- Some Common Time-Based Coding Errors (and How to Correct Them)
- Telehealth and Critical Care: How Time-Based Coding Applies
- EHR and Compliance: Smarter Time Tracking for Providers
- The Time-Based Audit Checklist for 2025
- How Time-Based Coding Improves Reimbursement and Efficiency
- Partner with Experts to Maximize Accuracy
- Conclusion
In 2025, time-based coding is a critical component of appropriate reimbursement and compliance in medical billing. If you are not capturing the data as such today, this analysis reflects an opportunity: Healthcare professionals across the US are moving toward clock-in/clock-out style documentation to prepare for updated CPT 2025 guidelines and prevent claim rejections. The shift is changing how provider effort, clinical accuracy, and care coordination are valued and paid for.
Mastering time-based coding is as important to physicians as it is to those who send the bills—for transparency, fairness, and value-based care. It allows providers to ensure every minute earned with their expertise is counted toward suitable reimbursement, bolstering compliance and financial success in today’s complex healthcare world.
What Is Time-Based Coding, and Why Does It Matter for Providers?
Time-based coding refers to the amount of time a provider spends on patient care—before, during, and after the visit. These activities include face-to-face counseling, discussing test results, recording findings, and coordinating care with other providers.
Historically, reimbursement focused on MDM (medical decision-making). Now, CPT 2025 lets providers bill for total patient encounter time. This change helps providers capture all their work, not just exam room time.
Source
Example Table: Face-to-Face vs Total Time (CPT Concept)
| Does Activity Type Count Toward Time? | Example |
| Face-to-Face Patient Interaction | Yes — Counseling, physical exam |
| Non-Face-to-Face Work | Yes — Reviewing labs, documentation |
| Staff-Only Work | No — Scheduling, vitals by nurse |
| Teaching or Travel | No — Non-billable |
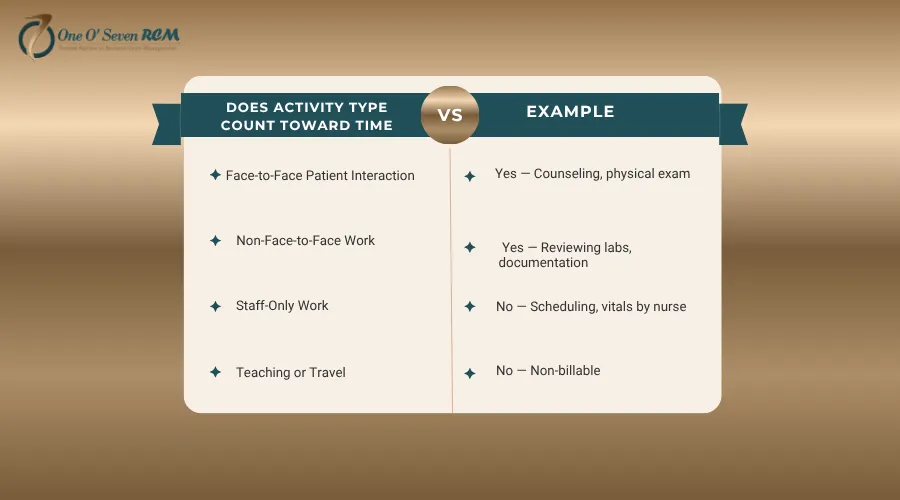
When documented correctly, time-based coding ensures your professional time is acknowledged—and compensated.
CPT 2025 Time-Based Guidelines: How Time Is Calculated
CPT 2025 now counts both direct and indirect care given on the same day as “total time.”
Reference
CPT Time Threshold Table (2025 Update)
| Patient Type | CPT Code | Time Range (Minutes) | Example Use |
| New | 99202 | 15–29 | Simple evaluation |
| 99203 | 30–44 | Moderate visit | |
| 99204 | 45–59 | Complex case | |
| 99205 | 60–74 | Comprehensive care | |
| Established | 99212 | 10–19 | Minor follow-up |
| 99213 | 20–29 | Moderate visit | |
| 99214 | 30–39 | Complex visit | |
| 99215 | 40–54 | Prolonged visit |
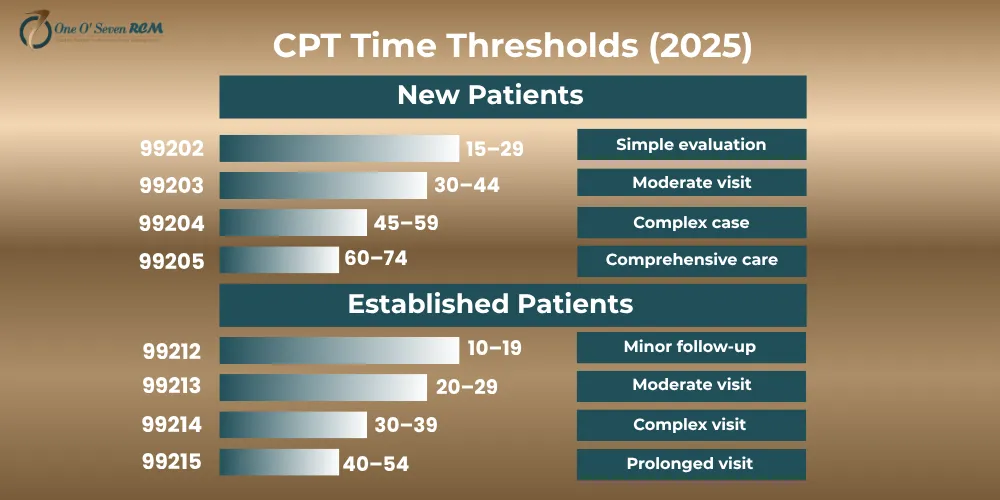
If your time exceeds the threshold, add prolonged service codes (99417, 99418) in 15-minute increments—just be sure to document the time accurately.
How Total Time Is Counted (and What Isn’t)
Not every minute counts. The trick lies in understanding which activities qualify toward total time:
Activities That Count:
- Reviewing patient charts and history
- Performing a medically appropriate exam
- Counseling and patient/family education
- Care coordination with other professionals
- Documenting clinical findings in EHR
- Ordering labs, tests, and prescriptions
Activities That Don’t Count:
- Time spent on separately billable procedures
- General teaching unrelated to the patient
- Travel or waiting time
- Work completed by nursing or administrative staff
If it’s not personally performed by the provider, it doesn’t count. Document what you do, not what your support staff does. That’s how you maintain both accuracy and compliance.
Time-Based Coding vs. MDM: When to Use Which
This is one of the most common questions among providers. Should you use time-based coding or stick with MDM?
Here’s the short answer:
- Choose time-based coding when your patient encounters are long and involve detailed counseling, charting, or coordination.
- Choose MDM-based coding when the case is driven by complexity rather than duration.
Practical Example:
You gave 40 minutes of counseling on lifestyle changes and medication adherence to a patient with hypertension.
The time-based route offers higher reimbursement than MDM, because counseling is your largest time investment.
Quick Comparison (in words, not table):
- Time-based: Duration-driven (how long you work)
- MDM-based: Complexity-driven (how hard the decision-making is)
- Time-based documentation favors extended visits
- MDM suits cases requiring critical decisions under pressure
Both methods have their place—switching appropriately helps you maximize payment.
Medical Billing
Best Practices for Documentation and Proper Billing
Good documentation protects you from audits and denials. Vague notes or forgotten timestamps can be costly.
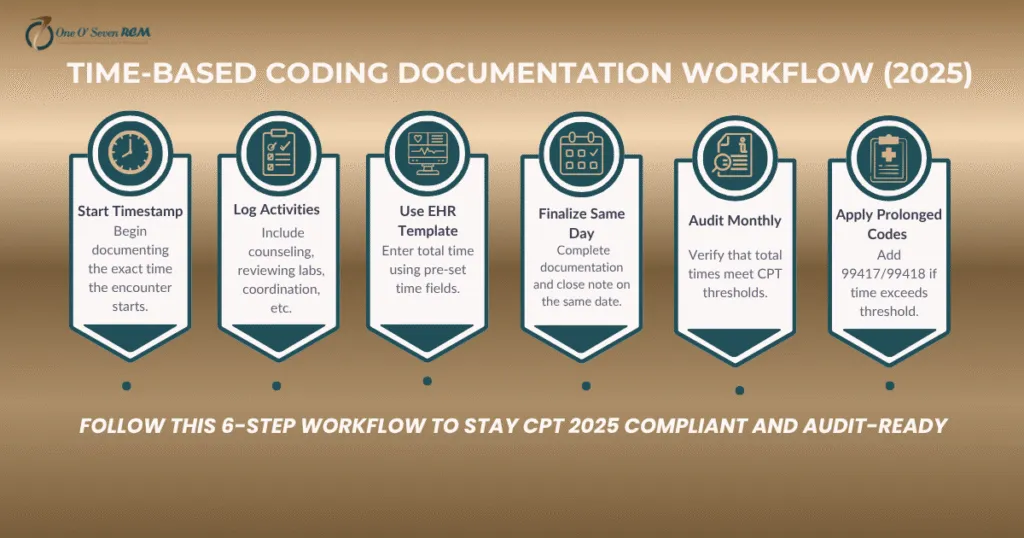
Here’s a bulletproof documentation workflow:
- Record start and stop times for every encounter.
- Describe activities in short, specific phrases (“Reviewed labs,” “Coordinated with cardiologist”).
- Avoid double-counting time spent on separately billable tasks.
- Add after-hours documentation if completed the same day.
- Use EHR templates that prompt for total time entry.
- Audit monthly to ensure alignment with CPT thresholds.
Pro Tip:
This saves time and gives you a strong audit trail.
Denial Management
Some Common Time-Based Coding Errors (and How to Correct Them)
Even experienced clinicians occasionally make small documentation errors, which can result in lost revenue. Let’s fix that.
Common Pitfalls and Fixes:
- Missing timestamps: Add automatic EHR stamps.
- Counting staff time: Only include provider-led work.
- Generic descriptions: Write specific activity summaries.
- Unclear total time: Record the sum clearly at the note’s end.
- Wrong CPT selection: Always reference the updated 2025 time ranges.
Auditors trust timestamps over memory. Precise documentation keeps your billing safe.
Telehealth and Critical Care: How Time-Based Coding Applies
Under CPT 2025, telehealth and critical care time-based billing now align with in-person processes if time is accurately recorded.
For telehealth, count time spent:
- Setting up a video connection
- Reviewing charts and lab results before the call
- Documenting after the session
- Counseling or patient education during the call
For critical care, count:
- All continuous bedside care
- Medical decision-making
- Documentation time on the same date
- Communication with family or specialists
Example:
A 90-minute sepsis stop time includes both direct patient care and charting. That’s CPT 99291 (first 74 minutes) + 99292 (next 16 minutes).
Use EHR logs for timestamps—they’re your best defense against audit.
EHR and Compliance: Smarter Time Tracking for Providers
EHR-integrated tools can automatically record and tag your time—so you focus on patients, not tracking.
Smart EHR Practices:
- Use “auto-log” features in platforms like Epic or Allscripts.
- Integrate TimeTag MD or Clockify Health to capture multitasking time.
- Schedule monthly audits—use your own timestamp logs for cross-verification.
Compliance Reminder:
CMS wants verifiable, real-time documentation. Let your EHR do the tracking so you focus on care.
Prolonged Services and Overlooked Minutes
Many providers miss out on prolonged service codes—use them if eligible.
If you exceed the top CPT threshold by at least eight minutes, bill one prolonged service unit (99417 for office visits, 99418 for inpatient visits).
Example:
A provider spends 68 minutes in an outpatient session coded 99215 (40–54 min range). The extra 14 minutes merit prolonged billing—one additional unit billed in compliance.
Each additional 15 minutes may seem minor, but over a series of visits, they can add significant revenue each year.
The Time-Based Audit Checklist for 2025
Here’s your quick internal audit guide.
Download and store this in your practice’s compliance folder.
Checklist Highlights:
- Start/stop times for every encounter
- Total time documented at note end
- Qualifying activities listed clearly
- CPT code matched to time threshold
- Non-face-to-face time included
- Documentation was completed the same day
- Separate procedures excluded
- Total time reviewed weekly
This is your payer review safety net: simple, reliable, CPT-compliant.
How Time-Based Coding Improves Reimbursement and Efficiency
Providers who master time-based coding typically see a 20–35% revenue increase. Why? Because they get paid for tasks they already do—charting, coordinating, reviewing results, and communicating care plans.
It’s not about overcharging payers—it’s about claiming what you’ve rightfully earned.
EHR automation, structured templates, and periodic self-audits can simultaneously enhance compliance and accuracy.
Mini Case Study:
A primary care clinic in Florida adopted a 7-step time documentation template through its EHR. Within 90 days:
- Denials declined by 28%
- Average revenue per visit increased by 22%
- Audit readiness improved across all payer categories
Time truly is money.
Partner with Experts to Maximize Accuracy
Effective time-based coding takes expertise. Billing partners can help.
One O Seven RCM collaborates with healthcare providers across the USA, helping them streamline EHR documentation, automate audits, and apply CPT updates flawlessly.
Their experts don’t just process claims—they train staff, build custom templates, and ensure every minute of your work translates into revenue.
Get in touch to receive your free 2025 Time-Based Coding Compliance Kit and boost your revenue integrity today.

Conclusion
Time-based Approach in a Changing Health Care Environment Today, time-based coding is not just an alternative method of reimbursement—it’s the driver that creates alignment between effort, documentation, and reward. You never know when you will need to defend the value of your clinical time, and CPT 2025 time-based coding standards allow providers to ensure they are capturing the full value of their clinical minutes (while maintaining accuracy).
Smart time-based coding enables providers to maximize compliance, reduce denials and be assured that all patient engagements, consults and follow-ups are properly reimbursed. The more rigorously you practice time entry and management, the stronger your revenue cycle becomes. As we enter the age of accountability and records-driven care, we need time-based coding to accurately capture the many hours therapeutic professionals spend on our clients.
FAQs
Q1. How to document time-based coding?
Recording total encounter time, ie start and stop times, including the activities performed (counseling, reviewing labs, coordinating care), is accurate coding documentation for time.
Q2. Which CPT codes are time-based?
Common time-based Codes Common CPT codes based on “time” are 99202–99215: Office Visits, 99291–99292: Critical Care and 99417–99418 Prolonged services (CPT® 2025 guidelines).
Q3. What is the difference between time-based coding and MDM-based coding?
Time-based coding correlates with the overall time of encounter with a patient, and MDM-based coding is grounded on the complexity of clinical decisions and the severity of the case.
Q4. Why is time-based coding important for providers in 2025? Time-based coding makes for fair reimbursement, less denial risk and an acknowledgement that EHR-induced compliance is a more standard part of the game.